This World AIDS Day, we celebrate the tremendous progress that has been made in response to the HIV/AIDS epidemic, with more than 20 million people living with HIV accessing life-saving antiretroviral treatment (ART) as of today. The incredible scale up of ART in developing countries, with affordable generic drugs widely available and the majority of countries now offering treatment to all people living with HIV, is the result of massive efforts on the part of national governments, treatment advocates, patient and community groups, public health organizations, originator and generic pharmaceutical manufacturers and donor agencies.
However with an estimated 37 million people living with HIV worldwide, there is still a long way to go until the epidemic is under control. Achieving global UNAIDS-set targets of 90 percent of people living with HIV knowing their status, 90 percent of those receiving treatment and 90 percent achieving viral suppression will require smarter strategies to test, treat and retain these many millions on treatment, and to prevent further infections.
For people living with HIV effective ART means taking a combination of antiretroviral drugs (ARVs) which together work to suppress the virus and allow you to remain healthy, active and living a full life largely undisrupted by the infection. These drugs must be taken every day to ensure the virus remains suppressed. Poor adherence to ART can lead to treatment failure, however many people struggle with adherence due to experiencing unpleasant side effects. When sick with malaria, experiencing vivid dreams or hallucinations may be acceptable for a few days as you recover and then stop taking medication. For HIV, treatment is life-long and such side effects may be too.
ARVs have improved tremendously since the first available drugs, and widespread access has saved many lives, however some of the most widely prescribed regimens in low and middle income countries are associated with common side effects. Some of these side effects can be extremely debilitating and include dizziness, hallucinations, and mental health problems, and certain drugs are associated with increased risk of suicide. In high income countries the majority of people living with HIV have access to newer, more tolerable alternatives available from originator pharmaceutical companies, since governments and patients can afford to pay relatively high prices for them. Governments in developing countries operate on very limited health budgets and rely on the availability of generic drugs to provide mass treatment programs. Every shilling, rand or rupee spent on more expensive treatment is one that cannot be spent on other urgent health priorities. This creates a disparity in the quality of treatment options available to you, depending on where you live.
The approval by regulators in 2013 of a new drug, Dolutegravir (DTG), generated significant excitement due to its improved efficacy – the drug suppresses the virus faster than alternatives – and lack of debilitating side effects. The product quickly became the most prescribed ARV in the United States, and use grew rapidly, and continues to grow, where it is available – mostly in high income countries.
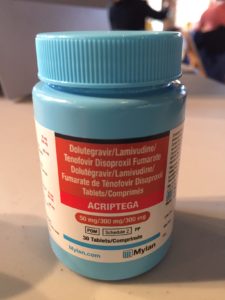
In September 2017, a groundbreaking announcement marked a huge step forward to providing equitable access to the best treatment options for people living with HIV in the developing world. The announcement at the UN General Assembly and the Global Citizens Festival means a once-daily combination of Tenofovir/Lamuviduine/Dolutegravir (TLD) will be widely available at a projected average of around $75 per person per year to 92 low- and middle-income countries. This is a treatment milestone as it is the first time the best available one pill, once daily regimen is available for a price lower than the most commonly used regimen. This means governments can achieve two often-conflicting priorities simultaneously: offering better treatment options to patients and reducing overall treatment costs to make limited budgets go further. The announcement was the result of efforts from a consortium of partners including Unitaid, Gates, CHAI, USAID, GF, WHO, UNAIDS, DFID, Mylan, Aurobindo, and ViiV along with the governments of South Africa and Kenya.
Since the announcement many countries have taken action to accelerate access to the TLD regimen. CHAI country teams are working with the governments in Kenya, Nigeria and Uganda through an initiative supported by Unitaid which enabled these countries to launch DTG in national treatment programs in mid-2017, generate experience of using the new drug amongst health care providers and patients, and pave the way to expedite availability of the TLD one pill, once daily regimen as soon as it was affordably available through the pricing agreement.
Salim, living in Kenya, is one of the first people in the country to access the new treatment. “Since the day I switched to DTG my overall health has greatly improved, and the drug has improved my quality of life”, he says. “I feel reenergized; my moods are even better now. I hope that policy makers and leaders will embrace and adopt Dolutegravir since it has been shown to be superior to many ARVs currently in our clinics. We need DTG now more than ever in Africa.”
Between now and the next World AIDS Day, millions of people in developing countries are expected to benefit from access to Dolutegravir. CHAI is working closely with many national programs and partners to make DTG accessible to patients. Beyond Kenya, Nigeria and Uganda, more than 30 low and middle income countries are preparing to make TLD available to their communities, including South Africa, which is home to around a third of people living with HIV. Kenly Sikwese, the Coordinator of the African Community Advisory Board representing people living with HIV (AfroCAB) and Chair of a CHAI-Unitaid Community Advisory Board focused on treatment optimization, has been advocating for rapid access to Dolutegravir for patients since its initial approval, and is excited about the prospect of widespread access.
“Many people living with HIV have reported remarkable improvement in their quality of life, with less side effects through taking DTG, giving us greater confidence of improved and better health status,” says Sikwese. “Widespread use of DTG could be the biggest game changer to impact the future of HIV care since the initial discovery of combined ART.”
Children often get left behind when there are advances in treatment. Formulations of new drugs that are suitable for children to take typically only get developed many years after adult versions. Children often suffer poor outcomes, partly as a result of their limited and poorly tolerated treatment options; better pediatric ARVs are desperately needed. CHAI is working to accelerate access to generic pediatric formulations of DTG to avoid delays in children benefitting from the new drug.
Dolutegravir access will go some way to improving treatment options for patients, helping people to adhere to treatment and maintain viral suppression. Effective treatment is one of the most critical strategies to reducing new HIV infections, since people who are virally suppressed are highly unlikely to transmit the virus. However, this is just one piece of the complex fight against the epidemic – we need better testing, more convenient ways of accessing treatment, better adherence and mental health support, and wider access to new prevention methods, such as oral pre-exposure prophylaxis (PrEP), to give people more options to protect themselves from infection. Sikwese says, “Dolutegravir means our best foot forward” – by World AIDS Day 2018, the world should be several more steps along the challenging and complex journey to bringing the epidemic to an end.
This work is funded through support from Unitaid and complementary funding from the UK Department for International Development.
More World AIDS Day coverage:
Blog: From volunteer to COO, working on Tanzania’s first-ever HIV/AIDS treatment plan
Blog: How ‘miracle’ of AIDS patients’ survival gives hope for future
The state of the antiretroviral market today
CHAI Access Program launches online HIV product toolkit






