Enormous progress has recently been made in the global fight against malaria, with over a billion malaria illnesses and six million malaria deaths averted over the past 15 years. Aiming to build upon this success, the World Health Organization has set ambitious targets of reducing malaria mortality and case incidence by an additional 40% by 2020. At the same time, many countries seek to go beyond burden reduction and eliminate malaria altogether, a goal which appears increasingly realistic in several regions of the world, including Central America, the Caribbean, and parts of Southeast Asia and Southern Africa.
Financing for malaria control now amounts to an impressive US $2.5B annually, but various estimates suggest that donor contributions will need to increase by 140%-250% to achieve our global malaria objectives. While more funding will almost certainly be required, it is critical that we in the malaria community strive to achieve more with the resources we already have. For example, we have estimated that about half of the US $250M in malaria drugs purchased by donors for endemic countries last year were consumed by people who do not truly have malaria: many received the drugs based on an incorrect suspicion of malaria rather than a positive result from a blood test. In places where malaria is – or used to be – common, there is often a presumption that having a fever means having malaria even though many other illnesses have similar symptoms. Taking unnecessary drugs may mean patients are not treated for the real underlying cause of their illness, while sufficient supplies of life-saving drugs are not available for those who truly need them. Overtreatment also obscures the fact that malaria transmission tends to be highly focalized to certain regions or communities, preventing malaria programs from deploying their limited resources as optimally as possible.
Similar inefficiencies occur with the distribution of bed-nets, a proven, cost-effective way to prevent malaria that has saved millions of lives and counting. We need more funding to buy more nets and save more lives, but we also need to use the nets we have as efficiently as possible. A recent analysis by Oxford University estimated that about one quarter of new nets may be over-distributed to households that already own enough of them, leading to around US $100M of international donor funding that is essentially wasted each year.
In other words, we’ve done well, but we can do better. At the Clinton Health Access Initiative, Inc. (CHAI), we work with national malaria programs to help them overcome these sorts of inefficiencies and achieve as much impact as possible from their available resources. For countries trying to eliminate malaria altogether—like Haiti, Guatemala, Botswana, Cambodia, and many others—improving the accuracy of data on when and where malaria cases occur can be a critical step towards identifying and excising the final places where transmission happens.
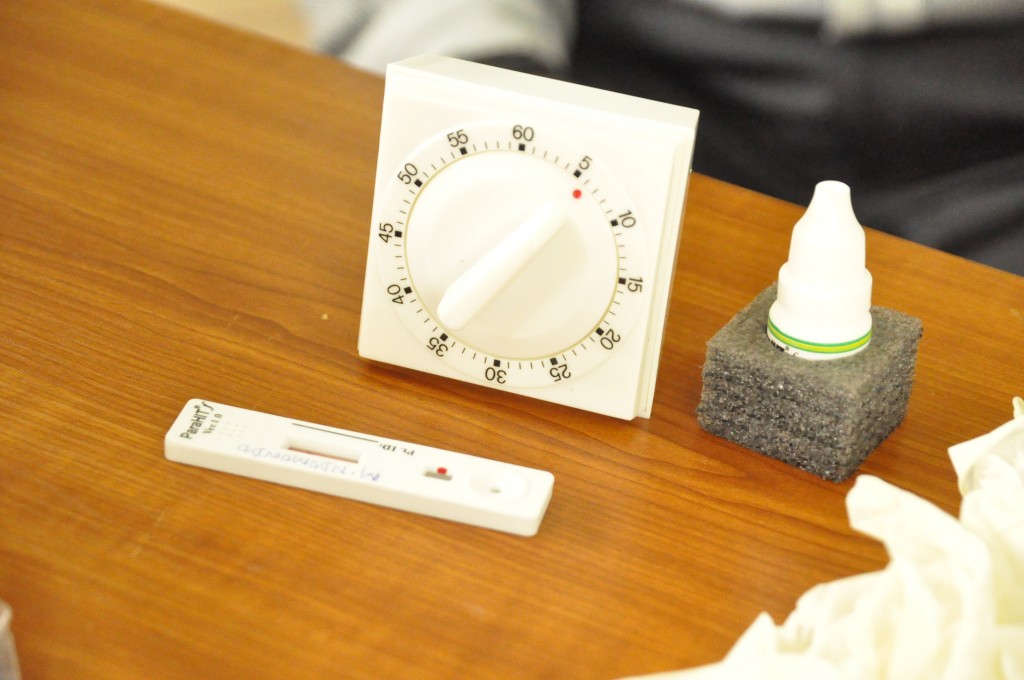
The first step towards building high-quality information systems for malaria elimination is to make sure all suspected malaria cases receive an accurate diagnosis. CHAI helps malaria programs scale up access to appropriate testing, in particular focusing on availability and appropriate use of rapid diagnostic tests, inexpensive devices that are relatively easy to use and that can provide an accurate diagnosis in only 15 minutes without the need for electricity or a laboratory. These simple tests have the potential to make a big difference particularly in remote places where it may take weeks to ship a blood sample to a laboratory and return the results. In many countries, we’ve seen first-hand how scaling up accurate diagnosis can result in dramatic declines in malaria – not because of any true changes in disease incidence, but rather because a lot of “malaria” was really caused by something else. In Namibia, for example, the 14,000 malaria cases reported in 2011 plummeted to fewer than 3,000 the next year – almost entirely thanks to enhanced diagnosis.
After ensuring that all suspected malaria cases are diagnosed, there’s additional work to be done to help countries improve the precision of malaria data for targeted decision-making. Many countries report malaria case data in aggregate: District A had 500 cases, while District B had 1,000. While this sort of information can be useful for understanding general patterns in malaria across the country, elimination requires more precision. We might, for example, train healthcare workers to start recording which village patients live in, or even to mark their household locations on a map. Fine-scale geographic information lets us go beyond knowing that a region of the country has malaria to understanding exactly where cases occur: moving from “you can get malaria around here” to “the malaria in this region is in the community located closest to that swamp.”
Mapping malaria isn’t the only additional step towards honing our malaria intelligence. What malaria elimination programs need to know is not just where they can find malaria infections, but where people are actually getting infected. In countries like Cambodia, for example, people may be bitten by parasite-carrying mosquitoes not around their homes, but while they are out in the forest working. We might identify lots of malaria-infected people in the community, but if we focus on trying to spray houses with insecticide, we won’t have any effect on transmission since it’s not really happening there. As an extreme example, think about the over 200 cases of malaria that were identified in New York City in 2014. Though malaria is present in the Big Apple, protecting New Yorkers with bed-nets would be a waste of money and effort because we know that all of those patients acquired their infections while traveling abroad in endemic countries.
CHAI is similarly helping malaria programs improve their knowledge about where their observed malaria is actually transmitted by mosquitoes by supporting them to train healthcare workers to investigate how, when, and where patients became infected. For example, clinic staff might ask about all of the places where that individual traveled in recent weeks, thereby learning if they made a trip to a nearby region known to have high rates of transmission. With this information we can see malaria patterns in even more detail, and we can focus our interventions on the places where they can truly have the greatest impact.
None of these improvements in disease intelligence are necessarily high-tech. As long as malaria cases are accurately diagnosed, investigated, reported, and mapped, malaria programs will have the information they need to make better decisions. That said, technology provides us with exciting opportunities to make this process easier. By helping countries replace paper forms with electronic data entry, for example, we’re helping reporting to become quicker and more accurate, allowing programs to act faster using the most up to date information. We are taking advantage of the increasingly ubiquitous coverage of mobile phone networks by having healthcare workers text-message diagnostic test results into surveillance systems, even from very remote places. By using satellite imagery and advanced statistical techniques, we can help programs predict places at high risk of malaria even if it hasn’t yet been observed there.
World Malaria Day is an opportunity to remind everyone that even though we have made historic progress against malaria, our job is not yet done. We require additional investment to keep advancing towards a world without malaria. But we should also make our own investments as a malaria community to ensure that all countries have the systems in place to know exactly when, where, and why malaria transmission happens. Only through this sort of intelligence can we be certain that every dollar we have available is spent on the most impactful interventions possible, which will in turn give donors even more reason to trust malaria programs with their funds. By building smarter, more targeted programs, CHAI and its partners will help governments build upon their successes and advance toward a malaria-free world.