Lesotho is a small, landlocked country surrounded by South Africa with a population of about 2 million people. It also has the second highest prevalence of HIV in the world, with 23 percent of the population infected. This high HIV prevalence is a key contributing factor in Lesotho having one of the lowest life expectancies globally, falling just shy of 50 years for both men and women.
In an effort to combat the disease, Lesotho became the first country in sub-Saharan Africa to adopt the World Health Organization (WHO)’s revolutionary “Test and Treat” strategy in April 2016. These new guidelines recommend immediate initiation of lifesaving antiretroviral therapy (ART) for all individuals who test positive for HIV. Previously, with the exception of pregnant women and children under the age of 5, patients were only placed on ART based on their disease progression, or CD4 count.
The WHO’s Early Release Guidelines, disseminated in September 2015, helped spur Lesotho to adopt the Test and Treat policy. These guidelines were based on clinical trials and observational studies which provided new evidence of the deleterious effects of uncontrolled HIV replication on non-AIDS defining illnesses like cardiovascular, kidney, and liver disease, several forms of cancer, and neurocognitive disorders. The research also showed no serious adverse effects from early ART initiation.
Test and Treat will play a crucial role in helping Lesotho achieve its ambitious goal of reaching UNAID’s 90-90-90 targets by 2030. Within these targets, 90 percent of all HIV positive individuals will know their status, 90 percent of those with a known HIV positive status will be on treatment, and 90 percent of those on treatment will have viral suppression.
In a country like Lesotho, the decision to adopt this transformational policy seems obvious, however substantial preliminary analysis and strategic planning had to be undertaken to ensure its feasibility and sustainability. The capacity of the health system’s core pillars – human resources, physical infrastructure, information systems, and financial resources – had to be scrutinized to confirm that they could support this transition and the many demands that came with it.
Some of the anticipated impacts of adoption of the policy included:
• More people routinely accessing services at health facilities, stretching the workforce;
• Increased spending on medication and commodities;
• Increased need for space to store more medication at health facilities;
• Increased capacity-building costs such as robust trainings to educate healthcare workers on the new policies, as well as trainings to strengthen stock management and reporting;
• Increased demands on laboratory service;
• Increased resources to strengthen national monitoring and evaluation.
During the strategic planning process, CHAI played a key role in quantifying the financial impact of Test and Treat. The Health Financing Team built upon their existing costing work in the National HIV Strategic Plan, where they costed all commodities and operations to understand the total funding needed to support the plan, by forecasting the increase in costs for HIV treatment with this new policy. Their findings determined that there would be no substantial funding gap since the country had initially set very ambitious treatment targets.These costs were in line with what would be needed to sustain Test and Treat.
In addition to financial analysis, CHAI has been working with other four partners, including the Ministry of Health, to gather evidence on the effectiveness of community-based testing in finding undiagnosed HIV positive individuals through the Mobilizing HIV Identification and Treatment Project (M-HIT). The outcomes of this project will inform the Ministry on best practices for alternative (not facility-based) methods of providing HIV testing and service delivery; in this case actually bringing services to the patients. Expanding testing and treatment services beyond the health facility are crucial in reaching those in the greatest need and closing the gap in achieving the 90-90-90 targets.
It has been one year since Lesotho implemented Test and Treat nationwide, and there is a lot to celebrate. Since implementation, there have been no major medication stock outs and no overwhelmed health facilities. Crucially, the public has strongly supported the new guidelines.
Lesotho is now closer than ever to achieving 90 percent testing coverage. A study of 85 facilities found that within the first quarter of adoption, the number of people tested for HIV nearly doubled from the previous quarter, from 25,808 to 51,381, and the number of people found HIV positive increased by 41 percent.[1]
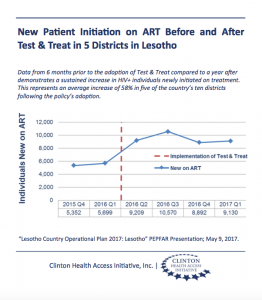
This increase in the number of patients tested similarly led to significantly more people starting ART. In 5 of the 10 districts in the country, an average increase of 58 percent of people initiating treatment was experienced throughout the first 10 months of Test and Treat compared to 8 months prior. The consistency of new patients starting treatment throughout the first year is proof that Lesotho’s heath system can and will sustain this policy change.[2]
Even with these successes, Lesotho’s ART coverage remains below 50 percent and there is still much work to do. However, with continued focus and responsiveness in adopting evidence-based approaches in eliminating HIV transmission and providing better treatment, Lesotho will win its battle against HIV.
[1] “Implementation Capacity Assessment Test and Treat Program in Lesotho” prepared by USAID, PEPFAR, and EQUIP; 2016
[2] “Lesotho Country Operational Plan 2017: Lesotho” PEPFAR; May 9, 2017





